|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
What Makes Pediatric Anesthesia Different?
Airway Airway Airway!!!
Infants and young children ARE NOT SMALL ADULTS.
There are Significant and Pertinent Anatomical and Physiological differences:
- HYPOXIA is the most common cause of pediatric perioperative cardiac arrest. INFANTS TURN BLUE FAST. UPPER AIRWAY OBSTRUCTION during anesthesia (particularly at induction and emergence) is a fairly common phenomenon.
- Complete and/or Partial LARYNGOSPASM is a fairly common problem
Infants and young children ARE NOT SMALL ADULTS.
- "One size fits all" DOES NOT APPLY.
There are Significant and Pertinent Anatomical and Physiological differences:
- Airway and Respiratory System
- Stages of Dentition
- Cardiovascular System
- Renal System
- Hepatic System
- Glucose Metabolism
- Hematology
- Temperature Control
- Central Nervous System
- Psychosocial
- Response to Pharmacologic Agents
Definitions
- Neonate / Newborn: A human offspring between ages 0 - 28 days of life. The term "neonate" is also used for all babies under 44 weeks PCA (post conceptual age)
- Infant: A human offspring between ages of 1 month and 12 months
- Toddler: Children between ages of 1 and 3 yrs
- Preschooler: Children between ages of 3-5 yrs
- School Age: Children between ages of 6-12 yrs
- Adolescent: 13 - 18 yrs
Airway and Respiratory System
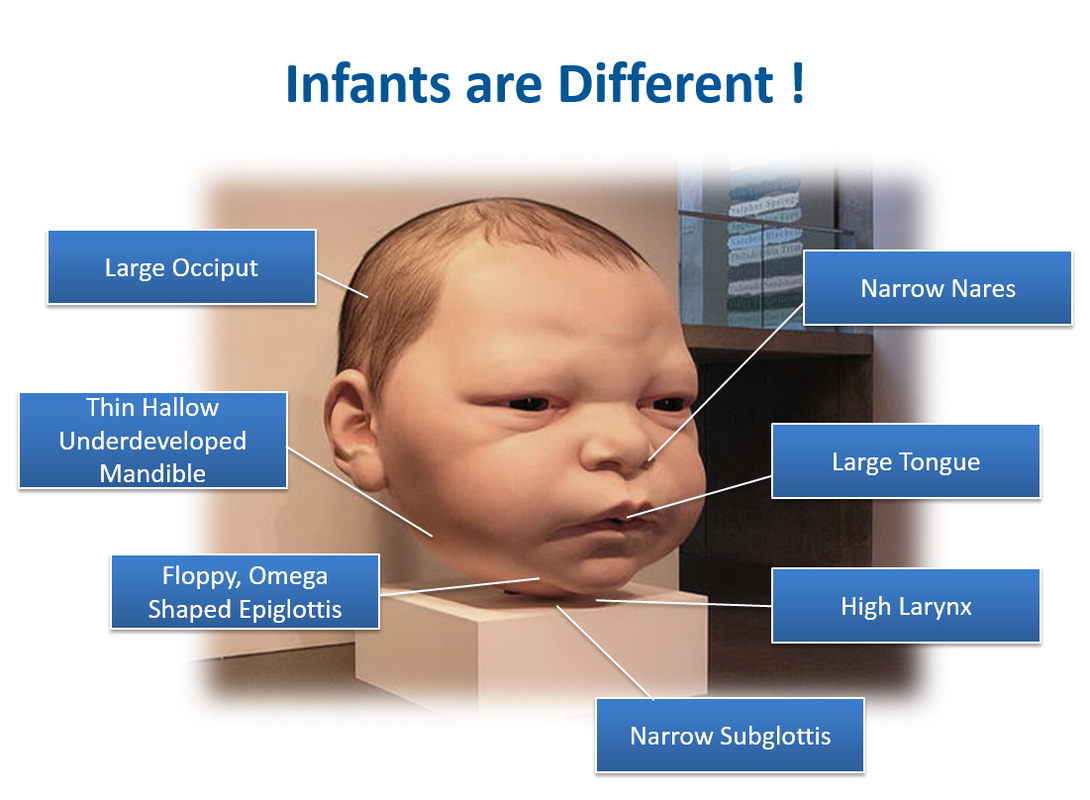
- Infants have a large head relative to their torso
- Tongue is relatively large and contributes to airway obstruction during anesthesia
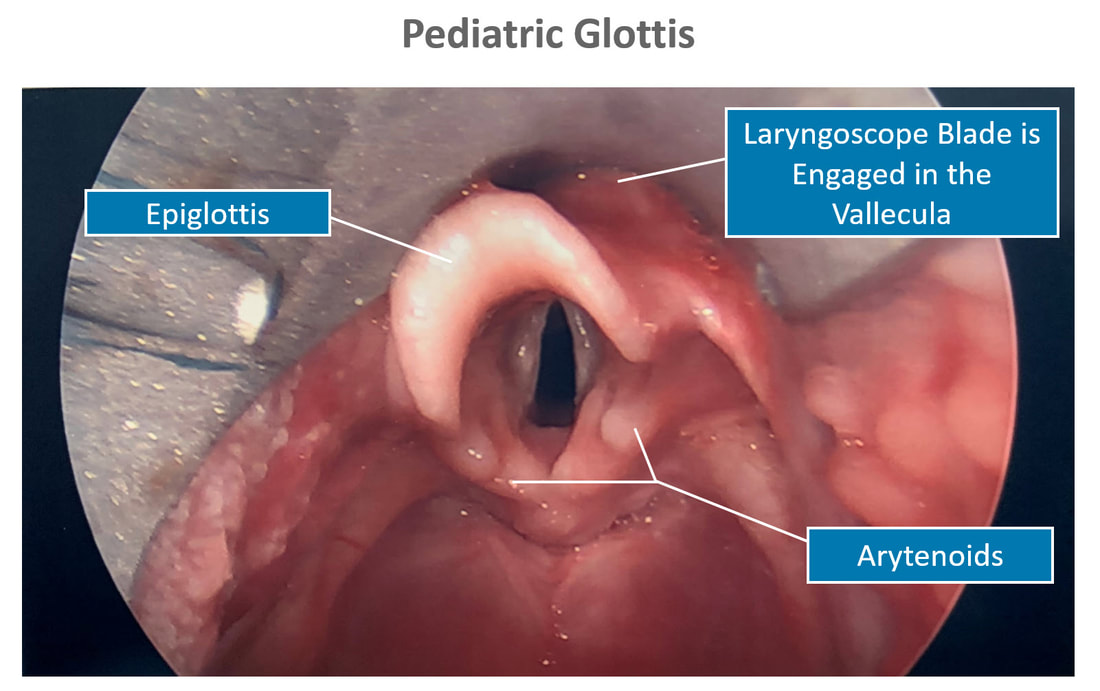
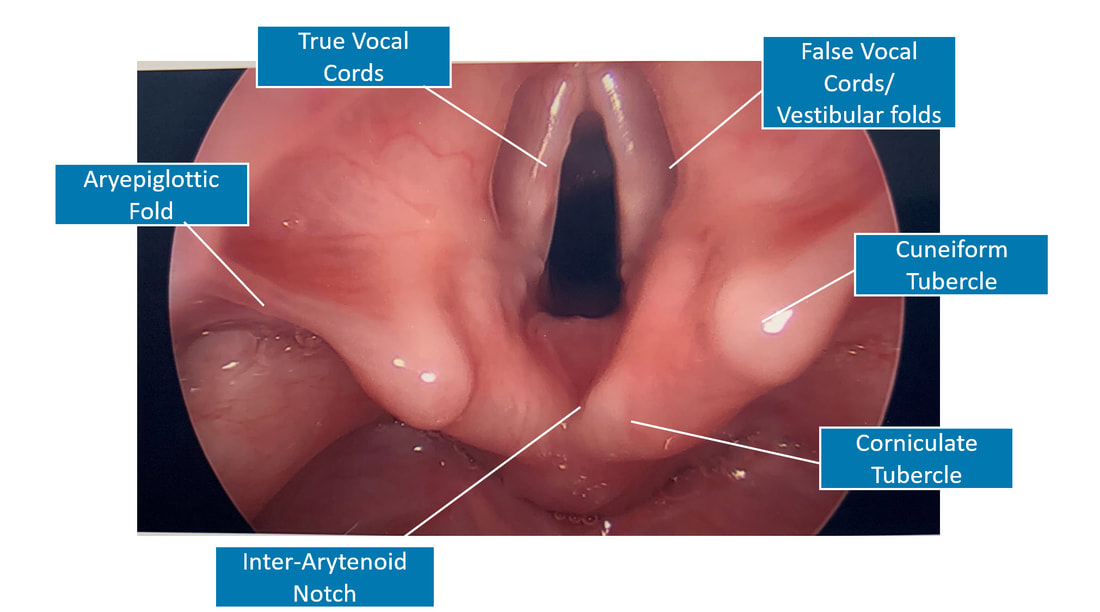
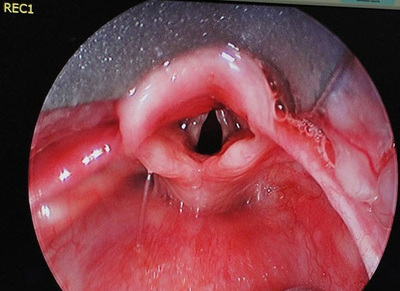
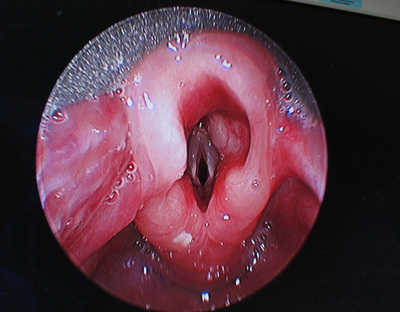
- The larynx is high and anterior, at the level of C3 - C4. The epiglottis is long, stiff and U-shaped. It flops posteriorly.
- Neonates and infants preferentially breathe through their nose. Their narrow nasal passages are easily blocked by secretions.
- The airway is narrowest at the level of the cricoid. Although there is ongoing debate whether this is true
- Infants have higher respiratory rates, low functional residual capacity (FRC), and higher work of breathing. Hence, neonates and infants fatigue faster.
- Postoperative apnea after anesthesia is common in very young infants (particulary premature infants). Please refer to the mandatory admission criteria page for additional information.
- Infants have higher oxygen consumption per kilogram of body weight
- Minute ventilation is more dependent on respiratory rate than on tidal volume
Stages of Dentition
Teething age of primary teeth:
- Central incisors : 6–12 months
- Lateral incisors : 9–16 months
- First molars : 13–19 months
- Canine teeth : 16–23 months
Cardiovascular System
The myocardium is less contractile in neonates causing the ventricles to be less compliant and less able to generate tension during contraction. This limits the size of the stroke volume. Cardiac output is therefore rate dependent. Bradycardia results in reduced cardiac output.
Please refer to the normal parameters section for additional detailed information.
Please refer to the normal parameters section for additional detailed information.
Renal System
Renal blood flow and glomerular filtration rate is low in the first 2 years of life due to high renal vascular resistance. They have lower tubular concentrating ability, which results in higher obligatory fluid loss.
Hepatic System
Liver function is initially immature with decreased function of hepatic enzymes. Barbiturates and opioids for example have a longer duration of action due to the slower metabolism.
Glucose Metabolism
Hypoglycaemia is common in the stressed neonate and glucose levels should be monitored regularly. Glycogen stores are located in the liver and myocardium. Neurological damage may result from hypoglycaemia. Please refer to the neonatal glucose requirements section for additional details.
Hematology
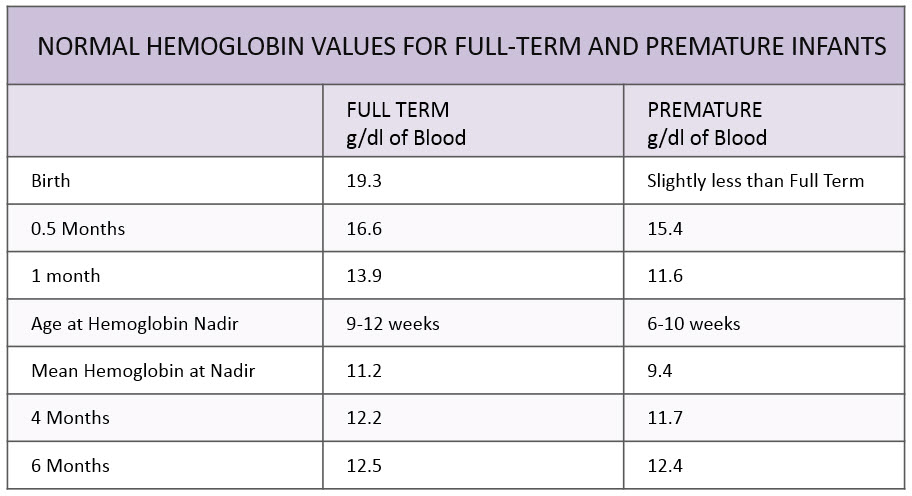
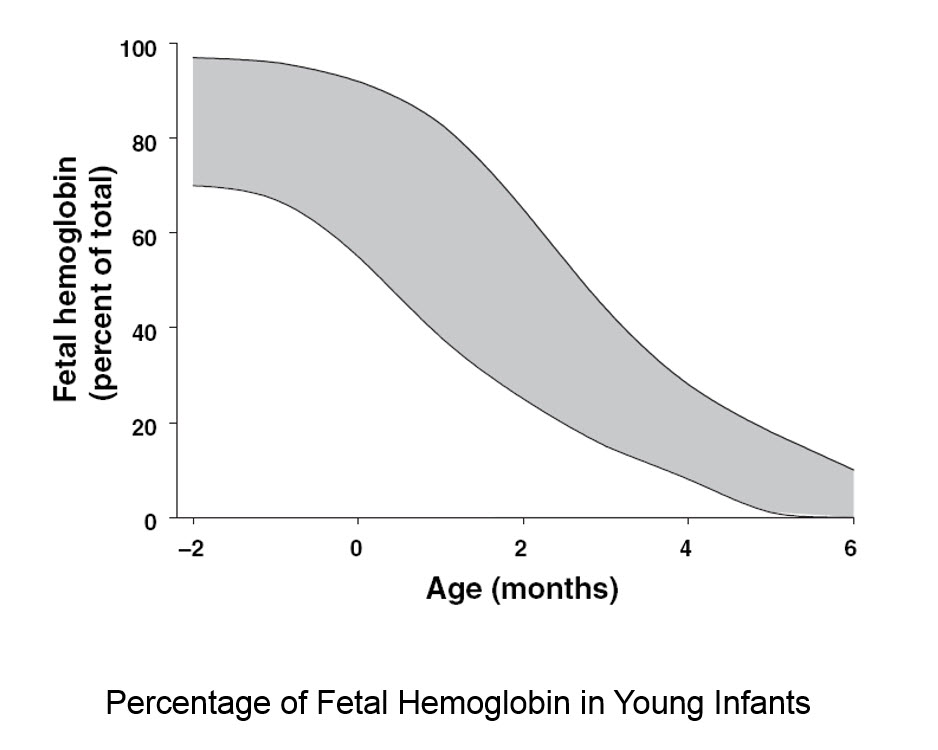
At birth, 70-90% of the hemoglobin molecules are HbF
Temperature Regulation
Babies and infants have a large surface area to weight ratio with minimal subcutaneous fat. They have poorly developed shivering, sweating and vasoconstriction mechanisms. Due to these reasons, heat loss is exaggerated during general anesthesia. Infants and children may lose up to 2 degrees (centigrade) during the first hour of anesthesia. Active measure must be taken to prevent heat loss. Forced air warming is among the best techniques to maintain body temperature during anesthesia. Warming IV fluids is also equally important.
Central Nervous System
A great deal of concern has recently arisen regarding the safety of anesthesia in infants and children. There is mounting and convincing preclinical evidence in rodents and non-human primates that anesthetics in common clinical use are neurotoxic to the developing brain in vitro and cause long-term neurobehavioral abnormalities in vivo. Over 150 articles have been published using animal models (from rodents to primates). All kinds of anesthetics (with the exception of perhaps xenon, and to some extent dexmedetomidine) have been implicated in neurotoxicity.
The difficulty in the interpretation of the clinical studies that have been completed to date is related to the retrospective nature of the studies, the lack of precise information in terms of age, agent, duration, and dose of anesthetics, specific agents used, the variable outcome endpoints used, and the way these outcomes were assessed. At present, results from in populo studies remain too sparse and too inconsistent to allow any recommendations for specific practice guidelines or changes in pediatric anesthesia practice. However, these studies do underscore the need for definitive studies in which outcome endpoints are specific and comprehensive, assessments are prospective and direct, and neuropsychological instruments used for assessment are validated and standardized.
The difficulty in the interpretation of the clinical studies that have been completed to date is related to the retrospective nature of the studies, the lack of precise information in terms of age, agent, duration, and dose of anesthetics, specific agents used, the variable outcome endpoints used, and the way these outcomes were assessed. At present, results from in populo studies remain too sparse and too inconsistent to allow any recommendations for specific practice guidelines or changes in pediatric anesthesia practice. However, these studies do underscore the need for definitive studies in which outcome endpoints are specific and comprehensive, assessments are prospective and direct, and neuropsychological instruments used for assessment are validated and standardized.
Psychology
Young Infants < 9 months are not usually upset by separation from their parents and will more readily accept a stranger.
Older Infants and children up to school age can get very upset and stressed by the separation from their parents and exposure to new unfamiliar people and surroundings. It is a challenge to rationalize with children of this age.
Older children and adolescents can get very apprehensive about the surgical procedure, its possible mutilating effects on their body, and the obvious possibility of pain. Older children are very concerned about loss of self-control and the unknown. The fear of not waking up after surgery can be very real and extremely disturbing for some children.
All these issues need to be tackled in an professional and artful manner. The ability and the need to build trust quickly with the child and his/her parent is extremely important skill-set for a pediatric anesthesiologist.
Checkout the CHILD LIFE section for additional information on this topic.
Older Infants and children up to school age can get very upset and stressed by the separation from their parents and exposure to new unfamiliar people and surroundings. It is a challenge to rationalize with children of this age.
Older children and adolescents can get very apprehensive about the surgical procedure, its possible mutilating effects on their body, and the obvious possibility of pain. Older children are very concerned about loss of self-control and the unknown. The fear of not waking up after surgery can be very real and extremely disturbing for some children.
All these issues need to be tackled in an professional and artful manner. The ability and the need to build trust quickly with the child and his/her parent is extremely important skill-set for a pediatric anesthesiologist.
Checkout the CHILD LIFE section for additional information on this topic.
Response to Pharmacolgic Agents
The extent of the differences among infants, children, and adults in response to the administration of drugs is not just a size conversion. During the first several months after birth, rapid development and growth of organ systems take place, altering the factors involved in uptake, distribution, metabolism, and elimination of anesthetics and related drugs.
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023