|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
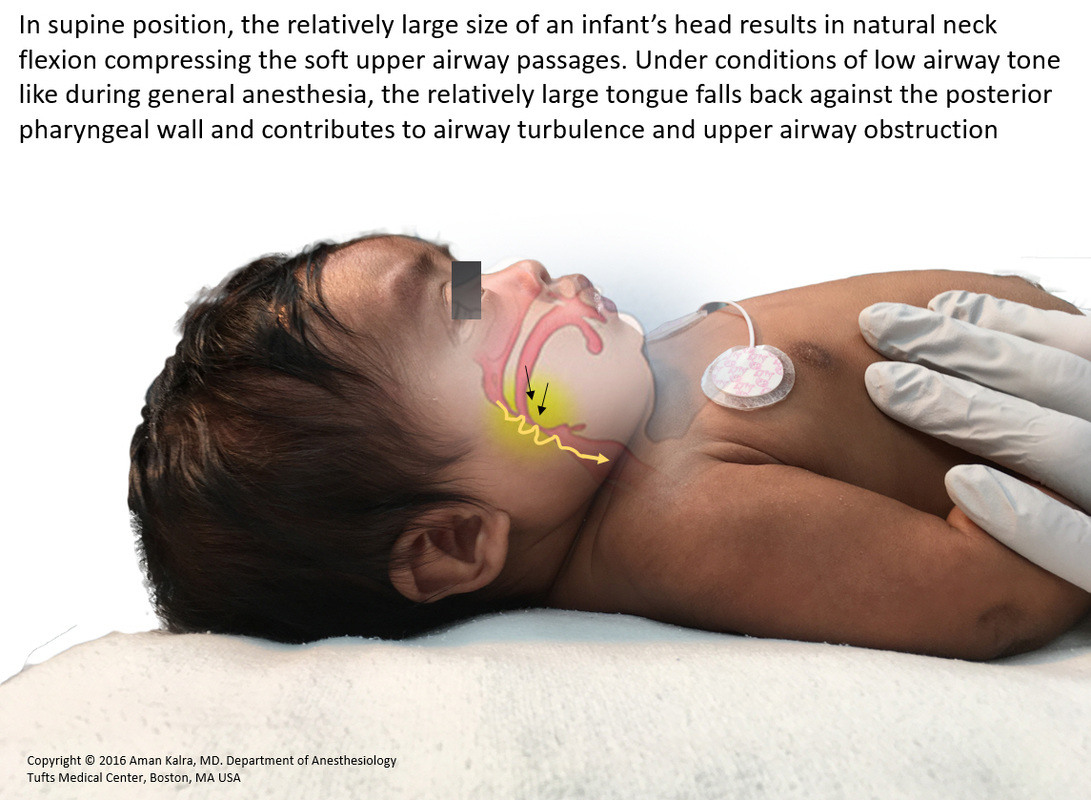
Upper Airway Obstruction During General Anesthesia
in Infants and Children
|
|
Upper airway obstruction during anesthesia particularly at times of induction and emergence is very common in infants and small children. Prompt management is critical in order to avoid oxygen desaturation and consequent hypoxemia. The following section summaries the causes and highlights proper clinical technique to manage this very fundamental problem in pediatric anesthesia
Check out the HD video presentation (on left) |
Signs and Symptoms
The hallmark of upper airway obstruction is diminished or absent airflow in the presence of continued respiratory effort. Complete upper airway obstruction is silent, while partial obstruction (the more common type) manifests as snoring and inspiratory stridor. Continued breathing effort against a partially or completely obstructed airway manifests it self as distorted paradoxical breathing and tracheal tug.
Genesis of Upper Airway Obstruction During Anesthesia
- Structurally the upper airway consists of a collapsible segment (nasopharynx, oropharynx and glottic and supraglottic larynx) situated in between two somewhat rigid tubes (nasal cavity and sub-glottis / trachea)
- Depressed and dysynchronous pharyngeal and laryngeal muscle tone during anesthesia (particularly during stage 2 of anesthesia (excitement stage)) results in collapse of naso-oropharyngeal soft tissue. This in turn decreases pharyngeal patency, increases turbulent air flow, and worsens upper airway obstruction
- Pediatric airway factors contribute immensely to upper airway obstruction. These include:
- Large head (An infant's large head relative to the trunk naturally flexes at the neck and compresses upper airway soft tissue)
- Large tongue (An infant's large tongue falls back into the posterior pharynx under conditions of depressed airway tone)
- Large and floppy epiglottis
- Excessive naso-oropharyngeal soft tissue
- Higher incidence of adenoidal and tonsillar hypertrophy in infants and children
- Partial / complete laryngospasm / laryngomalacia / chest rigidity and breath-holding are other factors which must be excluded
- Congenital airway anomalies like micrognathia, macroglossia, mid-facial hypoplasia can complicate airway management
Methods to Overcome Upper Airway Obstruction and Maintain Upper Airway Patency
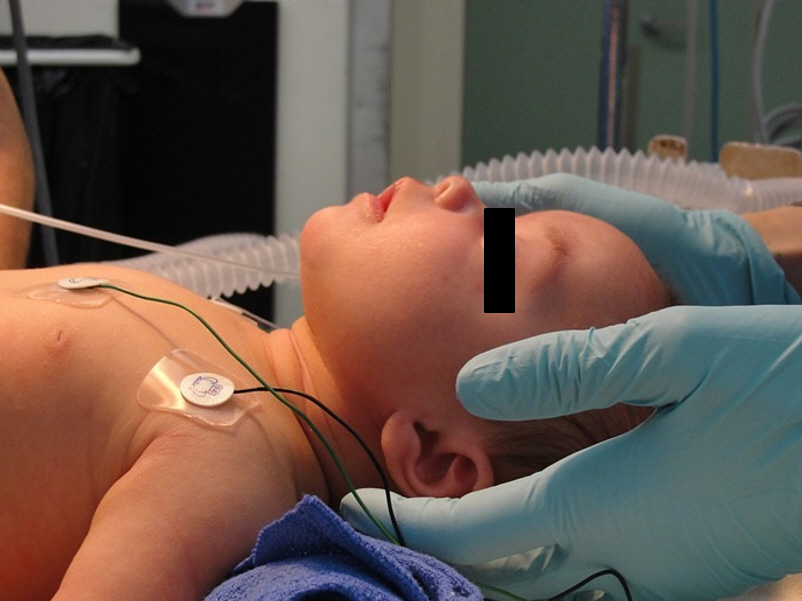
Optimal positioning utilizing both a shoulder roll and head rest is extremely important (see section of patient positioning). Sniffing position lines up the pharyngeal and laryngeal axis and helps to increase the available retropalatal and retroglossal spaces.
Triple Airway Maneuver:
1. Neck Extension
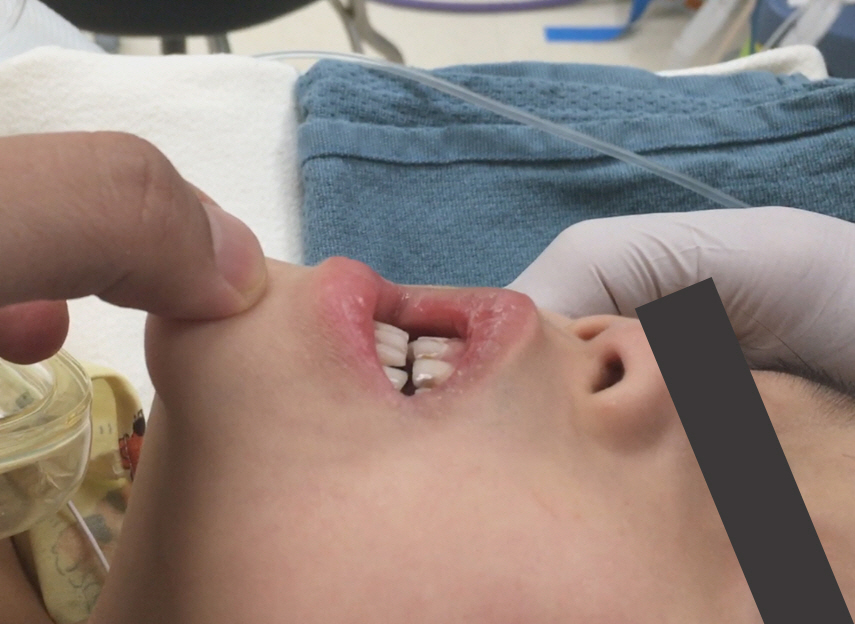
2. Jaw Thrust / Chin Lift
3. Mouth Opening
CPAP (Continuous Positive Airway Pressure) can help stent the airway open by counteracting the collapsing forces on the relaxed upper airway
Insertion of an Oropharyngeal / Nasopharyngeal Airway
Exclude and if needed treat partial / complete laryngospasm
Increase Depth of Anesthesia
Consider inserting a LMA
Triple Airway Maneuver:
1. Neck Extension
2. Jaw Thrust / Chin Lift
3. Mouth Opening
CPAP (Continuous Positive Airway Pressure) can help stent the airway open by counteracting the collapsing forces on the relaxed upper airway
Insertion of an Oropharyngeal / Nasopharyngeal Airway
Exclude and if needed treat partial / complete laryngospasm
Increase Depth of Anesthesia
Consider inserting a LMA
Neck Extension and Jaw ThrustPlace the thenar eminence of each hand on the side of the patient's head, near or just superior to the zygomatic arch, and then place the tips of your index finger under the patients angle of the mandible. While tilting the patient's head back, gently displace the jaw upwards and anteriorly (see images to the left), subluxating the TMJ in the process.
|
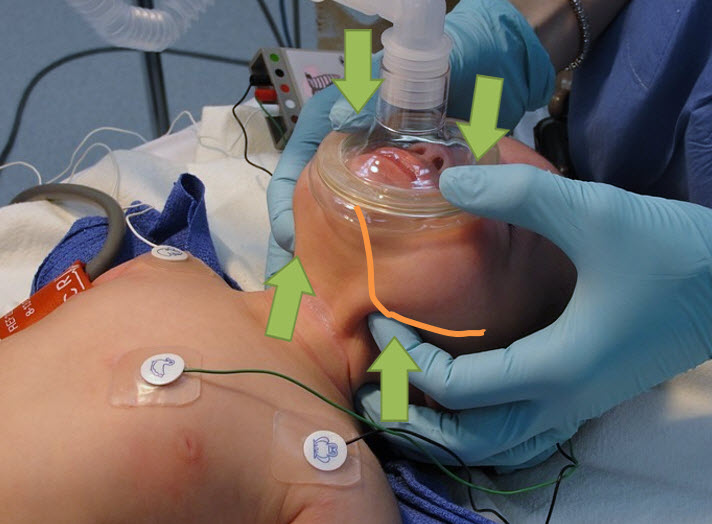
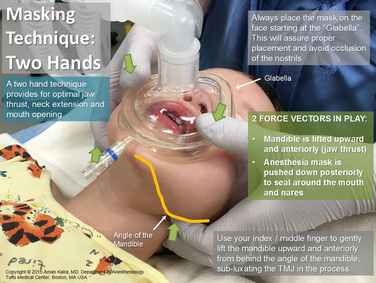
Jaw Thrust and Neck Extension with the Anesthesia Mask firmly over face using 2 Hand TechniqueNotice the placement of the mask. The nostrils are patent and without pressure. Use your thumb to hold the anesthesia mask tightly on to the face
Notice, how the face is being squeezed between the index finger and the thumb in this 2 hand technique. We have two force vectors in play - The mandible is being lifted anteriorly and the anesthesia mask is being forced down posteriorly over the face to create a good seal. It is hard to achieve adequate jaw thrust using a single hand technique The Two Force Vectors in Play while providing Jaw ThrustNotice, how the face is being squeezed between the index finger and the thumb in this 2 hand technique. We have two force vectors in play - The mandible is being lifted upwards and anteriorly and the anesthesia mask is being forced down posteriorly over the face to create a good seal.
The nares are not occluded and the mouth is slightly open It is hard to achieve adequate jaw thrust using a single hand technique |
|
|
Pediatric Jaw Thrust Video 1 |
|
|
Pediatric Jaw Thrust Video 2 (Tufts) |
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023