|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
Perioperative Fluid Therapy in Infants and Children
There are 2 Main Components of Perioperative Fluid Therapy:
- Maintenance Fluid and Electrolyte Therapy
- Restoration or Replenishment Fluid Therapy
Maintenance Fluid Therapy
Represents the fluid and electrolyte requirements needed by the average individual with normal intracellular(ICF)and extracellular(ECF) fluid volumes OVER a 24-hr PERIOD.
Major Objectives of Maintenance Fluid Therapy include:
Major Objectives of Maintenance Fluid Therapy include:
- Provide WATER to meet physiologic needs/losses
- Provide essential ELECTROLYTES (Na, K, Ca)
- Provide minimum CALORIC needs
Infants have HIGHER fluid requirements:
- Higher Rates of Metabolism and Growth
- Greater Caloric Expenditure translates into Higher Fluid Requirements
- Higher Insensible Fluid and Electrolyte losses due to a Greater Body Surface Area-to-Weight Ratio (almost
- 3 times)
- Lower Tubular Concentrating Ability, results in higher obligatory fluid loss.
- Higher Respiratory Rates result in higher insensible losses
Restoration or Replenishment Fluid Therapy
Represents restoration of circulatory volume by expanding extracellular fluid. Replenishment fluid therapy aims to replace body fluids and electrolytes lost through bleeding, fluid shifts and/or other pathological processes.
There are 2 major components of replenishment fluid therapy
There are 2 major components of replenishment fluid therapy
- Replacement of deficits incurred during preoperative fasting, GI preps etc.
- Replacement of ongoing extracellular losses. These primarily include shed blood loss, third space loss and evaporative loss. Extent of these losses depend on severity of surgical and non-surgical tissue trauma
Choice of Intravenous Fluids
There are several factors which determine, the choice, volume and combination of intravenous fluids to be administered in the perioperative environment. These predominantly include the following:
Until fairly recently (early - mid 1990s), hypotonic, dextrose containing fluids were primarily selected to restore circulating volume in infants and children in the perioperative environment. However, as clinical research has established the risks and perils of hyponatremia and hyperglycemia, the recommendations have changed over the last decade. Clinicians have realized, that most of the perioperative losses consist of isotonic extracellular fluids like shed blood, and interstitial fluids which are rich in sodium and chloride.
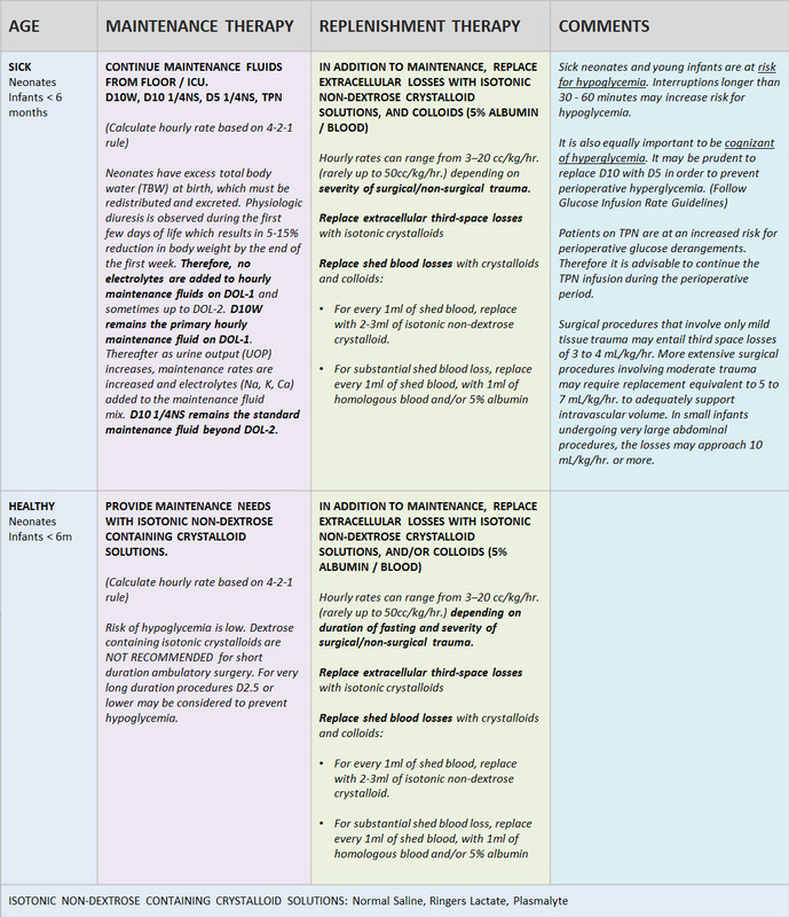
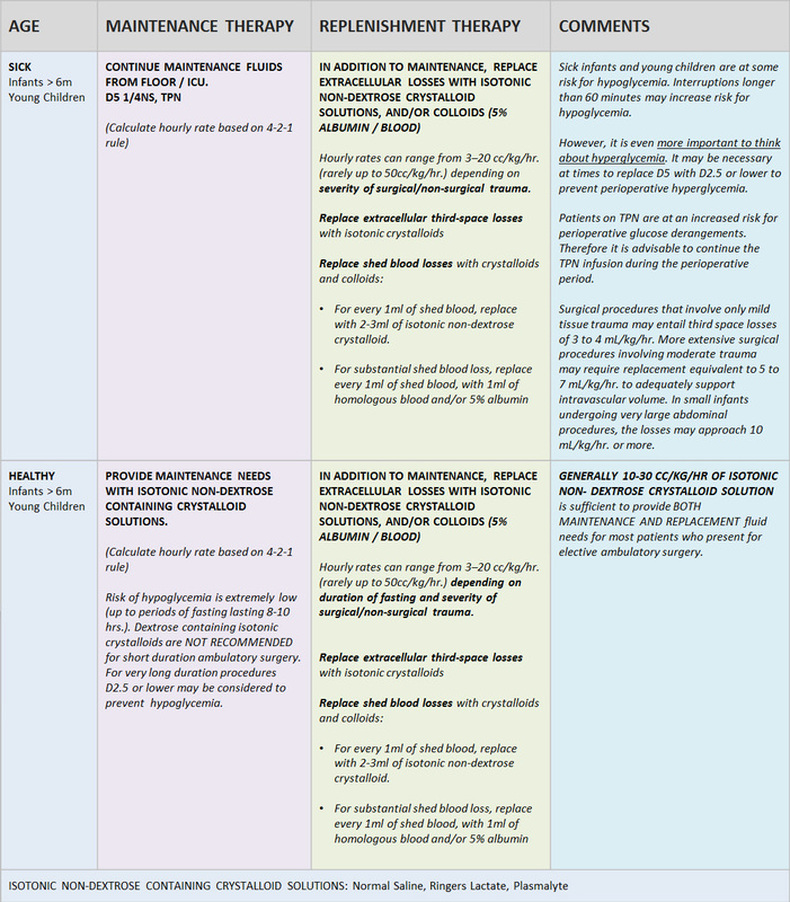
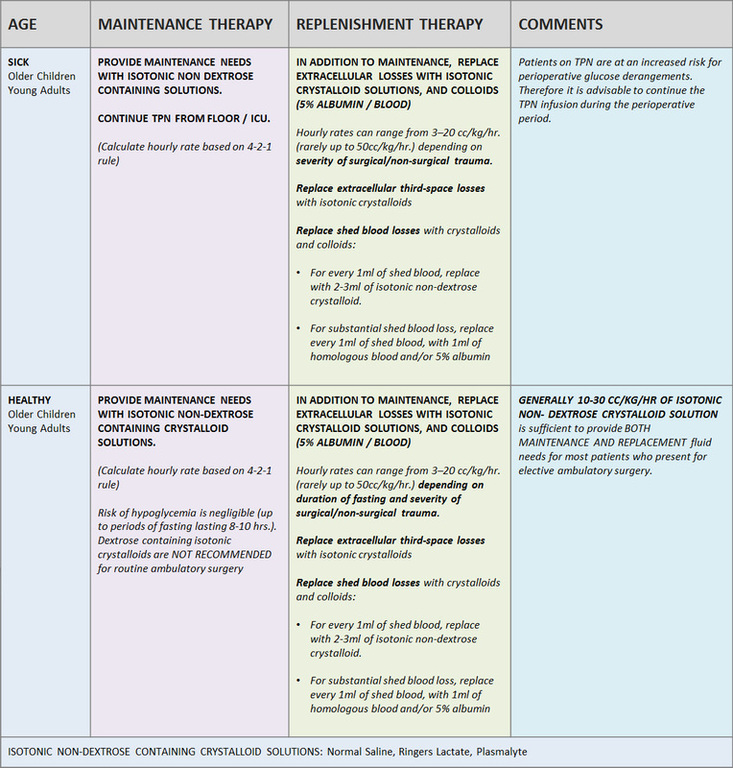
The following 3 tables summarize our recommendations for perioperative fluid therapy in neonates, infants, children and young adults:
- Age of the patient
- Nutritional status and Mandatory Glucose Energy Requirements
- Level of cellular injury and trauma
- Type and volume of ongoing fluid losses and/or fluid shifts
Until fairly recently (early - mid 1990s), hypotonic, dextrose containing fluids were primarily selected to restore circulating volume in infants and children in the perioperative environment. However, as clinical research has established the risks and perils of hyponatremia and hyperglycemia, the recommendations have changed over the last decade. Clinicians have realized, that most of the perioperative losses consist of isotonic extracellular fluids like shed blood, and interstitial fluids which are rich in sodium and chloride.
The following 3 tables summarize our recommendations for perioperative fluid therapy in neonates, infants, children and young adults:
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023