|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
|
Vertical Divider
|
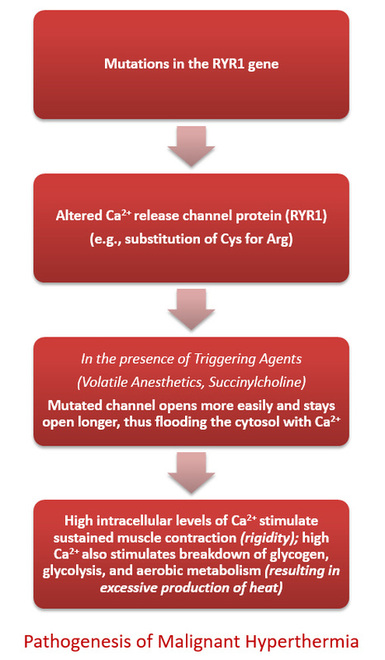
Malignant Hyperthermiais a pharmacogenetic disease of skeletal muscle that may precipitate a potentially fatal sequence of metabolic responses in the presence of triggering anesthetics. The primary triggers for MH are - Inhalational Anesthetics and Succinylcholine.
Incidence estimated at 1:10,000 and 1: 150,000. Etiology involves the uncontrollable release of intramyoplasmic calcium (Ca2+) that results in sustained muscle contractures, which in return produces a hypermetabolic response. The hypermetabolic response manifests as hypercarbia, hyperthermia, tachycardia, and if not treated early, a mixed metabolic and respiratory acidosis, muscle rigidity, severe rhabdomyolysis, circulatory shock and possibly death. NEW MH POLICY Updated FEB 2019:
(incorporates Ryanodex - a new dantrolene formulation) |
Anesthesia Workstation Preparation for MH Susceptible Patients
The recommended instructions for clearing residual anesthetic gases from our Drager Apollo Workstation include:
OPTION 1
OPTION 2
If time is of the essence, "Vapor-Clean" Activated Charcoal Filters may be used to quickly sanitize and prepare the machine for a vapor free anesthetic. Filter is effective in keeping gas concentration below 5 ppm for up to 12 hrs with FGF of at least 3L/min.
Instructions can be downloaded here
Instructional Video (requires Flash)
OPTION 1
- Remove vaporizer or disable by taping in OFF position
- Attach a new breathing circuit and reservoir bag to the Y-piece of the circle system and set the ventilator to inflate the bag periodically.
- Run Oxygen FGF at 10L/min with ventilator running, tidal volume of 600ml, rate of 10 breaths/min (1:2) for up to 104 minutes. For Drager Apollo the recommendation is 90 minutes for Isoflurane, and 50 minutes for Sevoflurane
- Changing CO2 absorbent is recommended
- Once the machine has been flushed, replace the breathing circuit with a new Breathing Circuit prior to Leak Test per recommended procedure.
- Machine is then ready for use!
OPTION 2
If time is of the essence, "Vapor-Clean" Activated Charcoal Filters may be used to quickly sanitize and prepare the machine for a vapor free anesthetic. Filter is effective in keeping gas concentration below 5 ppm for up to 12 hrs with FGF of at least 3L/min.
- Procedure requires flushing machine at high flow (>10L/min) for 90 seconds prior to placing filters on BOTH the inspiratory and expiratory ports.
Instructions can be downloaded here
Instructional Video (requires Flash)
The Malignant Hyperthermia Cart
|
Vertical Divider
|
The Cart is stored behind the Fish Bowl Nursing Desk in the F5 Main OR
|
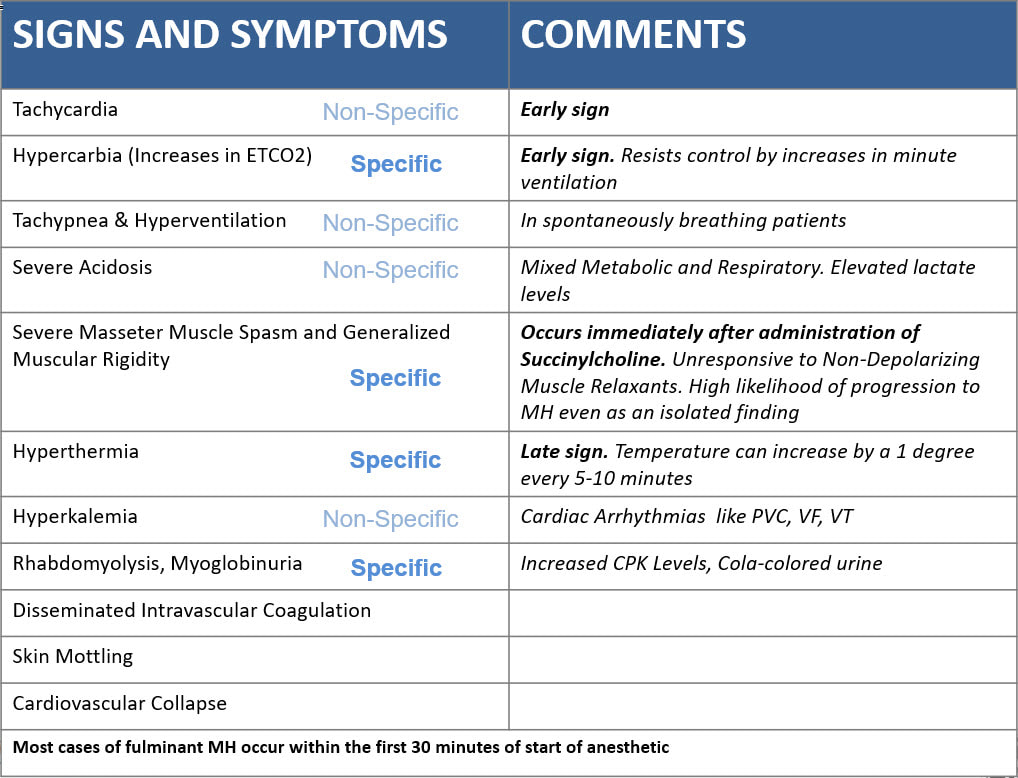
Clinical Presentation of MH
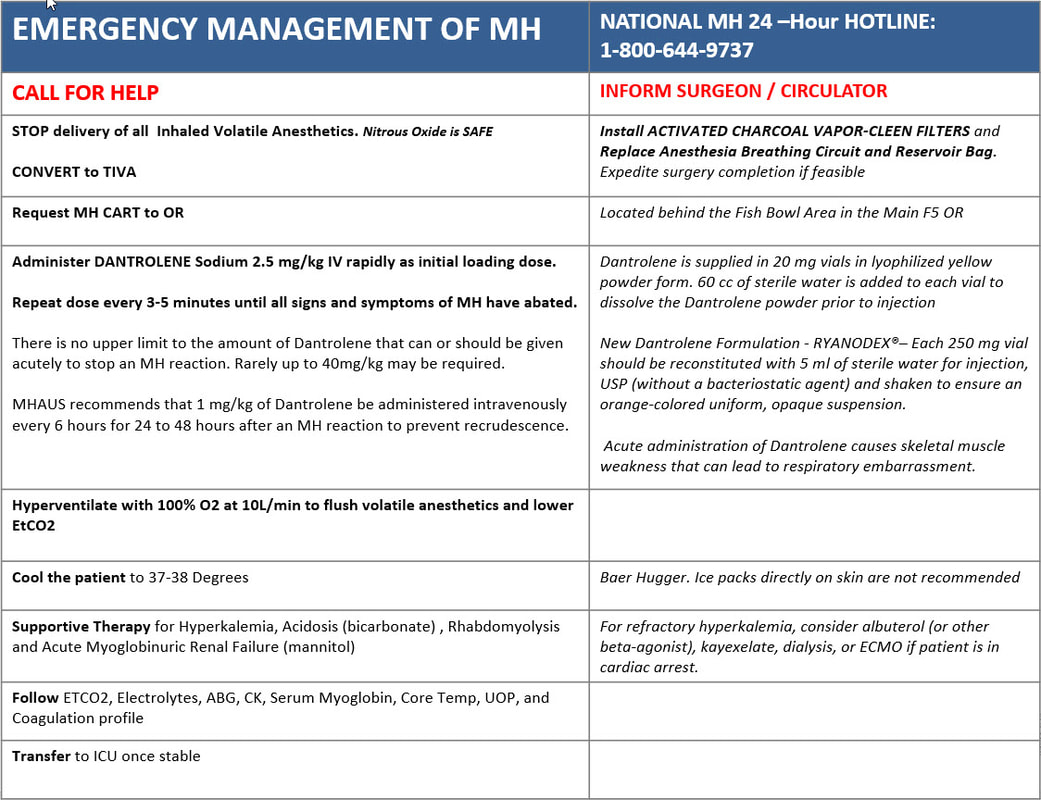
Management of Malignant Hyperthermia
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023