|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
Background
One of the primary objectives of maintenance parenteral fluid therapy is to provide water to meet physiologic losses (insensible loss + urine loss). In a study published in 1957, in the Journal Pediatrics, Malcolm Holliday and William Segar developed a simple scheme which could be easily remembered to calculate the maintenance water needs in hospitalized patients.
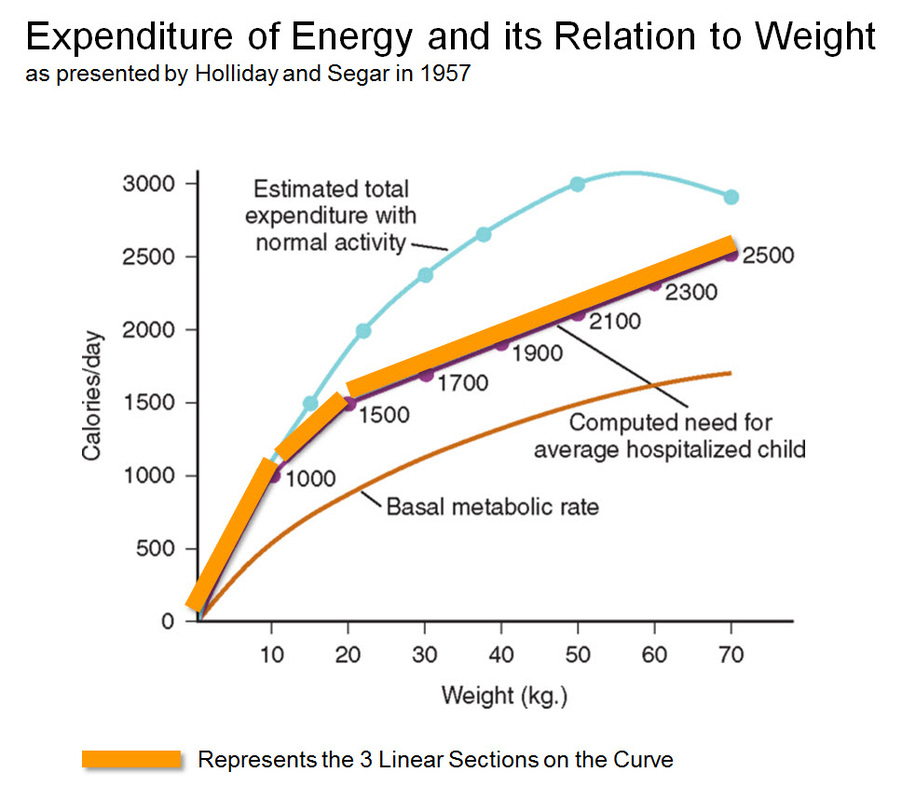
Assimilating the known physiology at the time, they observed that “there was a DIRECT LINEAR relationship between Physiologic Water Needs (insensible losses + urinary losses) and Energy Metabolism". In other words “the average needs for water, expressed in milliliters, equals energy expenditure in calories (under normal resting conditions, 1 ml of water is required to metabolize 1 kcal)".
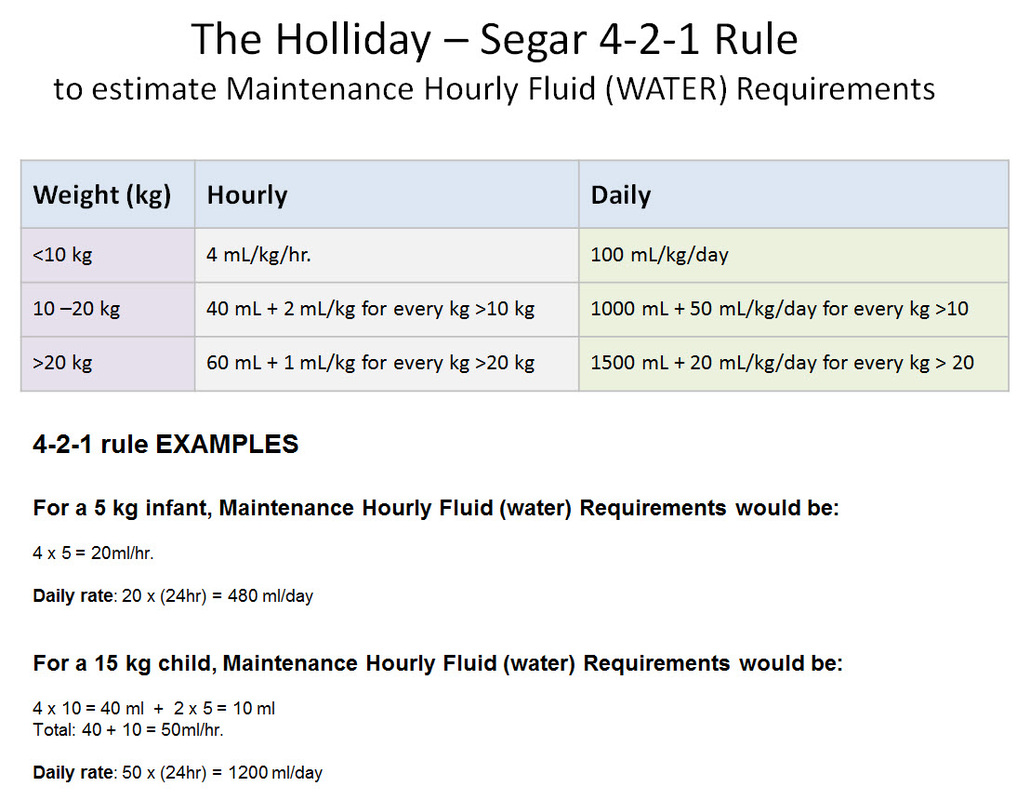
The relationship between Weight and Energy Expenditure was found to be NON-LINEAR. Based on their data and assumptions, Holliday and Segar constructed a curve plotting Energy Caloric Requirements versus Weight. This curve could be seen comprising of three linear sections which coincided approximately with the following weight sections: 0 to 10 kg, 10 to 20 kg, and 20 to 70 kg. Viewed in this manner, the authors concluded that 100 mL/kg/day for weights to 10 kg, an additional 50 mL/kg/day for each kilogram from 11 to 20 kg, and 20 mL/kg/day more for each kilogram beyond 20 kg. In anesthetic practice, this formula has been further simplified, with the hourly requirement referred to as the “4-2-1 rule” (4 mL/kg/hr for the first 10 kg of weight, 2 mL/kg/hr for the next 10 kg, and 1 mL/kg/hr for each kilogram thereafter.
Assimilating the known physiology at the time, they observed that “there was a DIRECT LINEAR relationship between Physiologic Water Needs (insensible losses + urinary losses) and Energy Metabolism". In other words “the average needs for water, expressed in milliliters, equals energy expenditure in calories (under normal resting conditions, 1 ml of water is required to metabolize 1 kcal)".
The relationship between Weight and Energy Expenditure was found to be NON-LINEAR. Based on their data and assumptions, Holliday and Segar constructed a curve plotting Energy Caloric Requirements versus Weight. This curve could be seen comprising of three linear sections which coincided approximately with the following weight sections: 0 to 10 kg, 10 to 20 kg, and 20 to 70 kg. Viewed in this manner, the authors concluded that 100 mL/kg/day for weights to 10 kg, an additional 50 mL/kg/day for each kilogram from 11 to 20 kg, and 20 mL/kg/day more for each kilogram beyond 20 kg. In anesthetic practice, this formula has been further simplified, with the hourly requirement referred to as the “4-2-1 rule” (4 mL/kg/hr for the first 10 kg of weight, 2 mL/kg/hr for the next 10 kg, and 1 mL/kg/hr for each kilogram thereafter.
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023