|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
OR SETUP - STEP 4
Prepare the OR Table and Positioning Props
A. Prepare the OR Table
For neonates, infants, and children, a Baer Hugger / Mistral Air Forced Air Warming Underbody Blanket should be placed securely on the OR bed. These come in two sizes - Neonate Plus and Large Pediatric Underbody. For older children and young adults, a regular upper or lower body Baer Hugger blanket should be considered.
The size of the operating bed may have to altered for neonates and infants. Communicate with your Attending Pediatric Anesthesiologist before making any alterations.
The size of the operating bed may have to altered for neonates and infants. Communicate with your Attending Pediatric Anesthesiologist before making any alterations.
B. Positioning Props
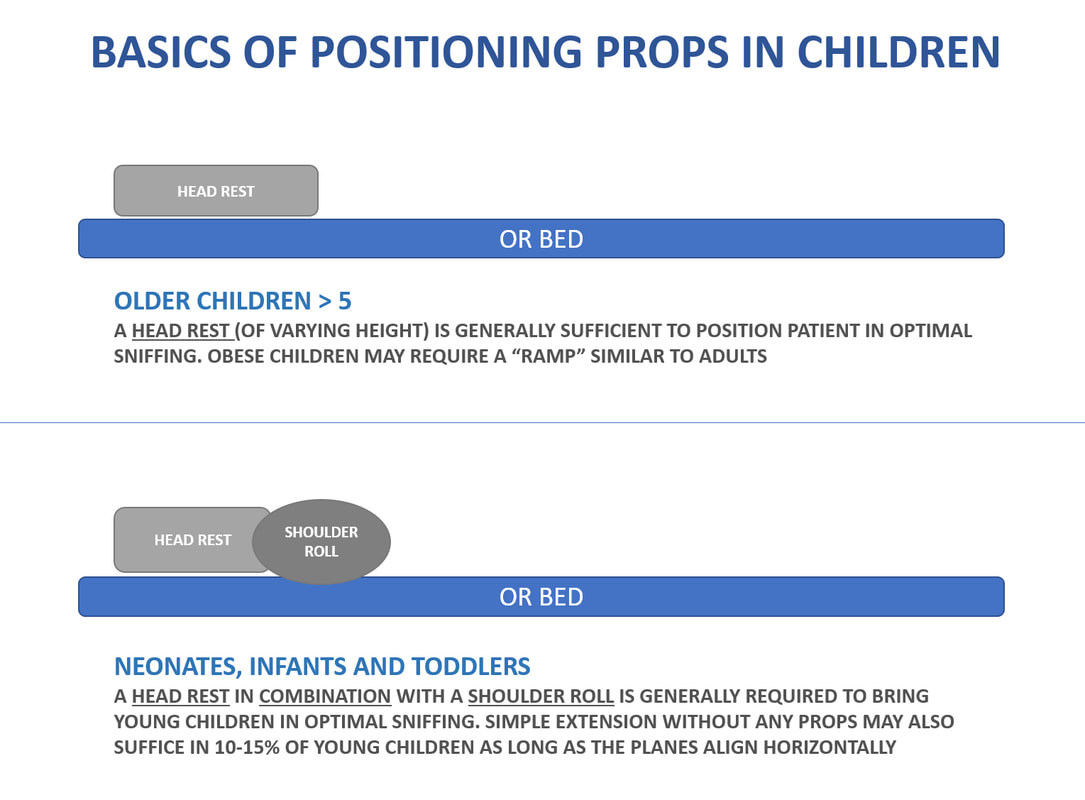
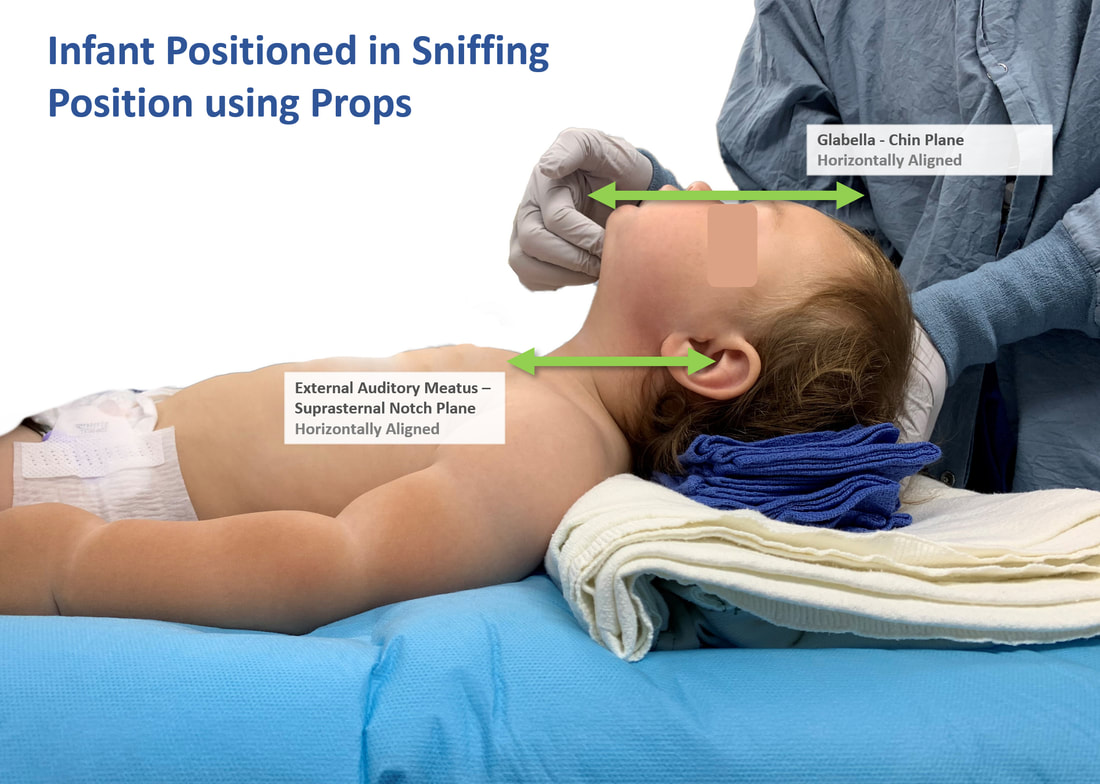
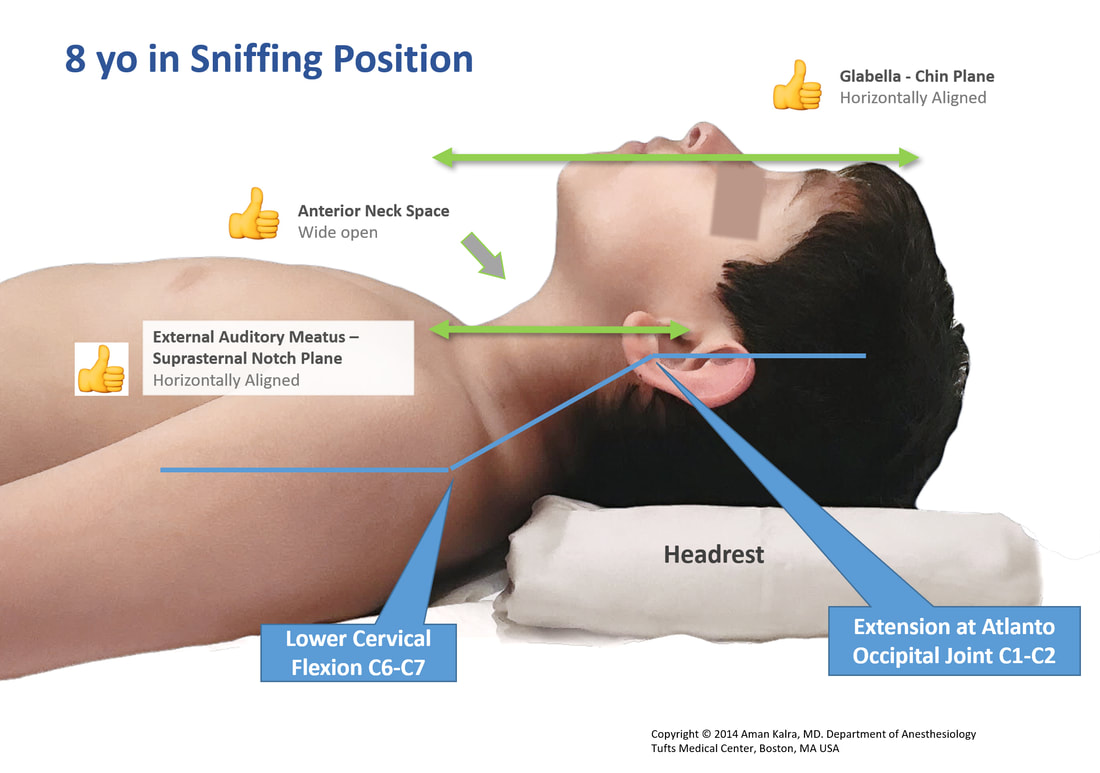
The classic sniffing position is an established standard across anesthesia practice. To bring children in the most optimal sniffing position, we must aim to align the External Auditory Meatus (EAM) in horizontal plane with the Suprasternal notch (SN). The Glabella - Chin face plane should also be near horizontal.
In older children, a head rest (of variable height depending on size of patient) is generally sufficient to achieve optimal sniffing. Older obese children may require ramping similar to practice in adults.
In infants and toddlers, a shoulder roll in combination with a head rest is recommended to optimally position for airway management. In a small proportion of infants and toddlers, simple head extension without any props may be sufficient to bring the planes in horizontal alignment.
Props can be created using different techniques and materials. the images below will demonstrate various common combinations.
In older children, a head rest (of variable height depending on size of patient) is generally sufficient to achieve optimal sniffing. Older obese children may require ramping similar to practice in adults.
In infants and toddlers, a shoulder roll in combination with a head rest is recommended to optimally position for airway management. In a small proportion of infants and toddlers, simple head extension without any props may be sufficient to bring the planes in horizontal alignment.
Props can be created using different techniques and materials. the images below will demonstrate various common combinations.
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023