|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
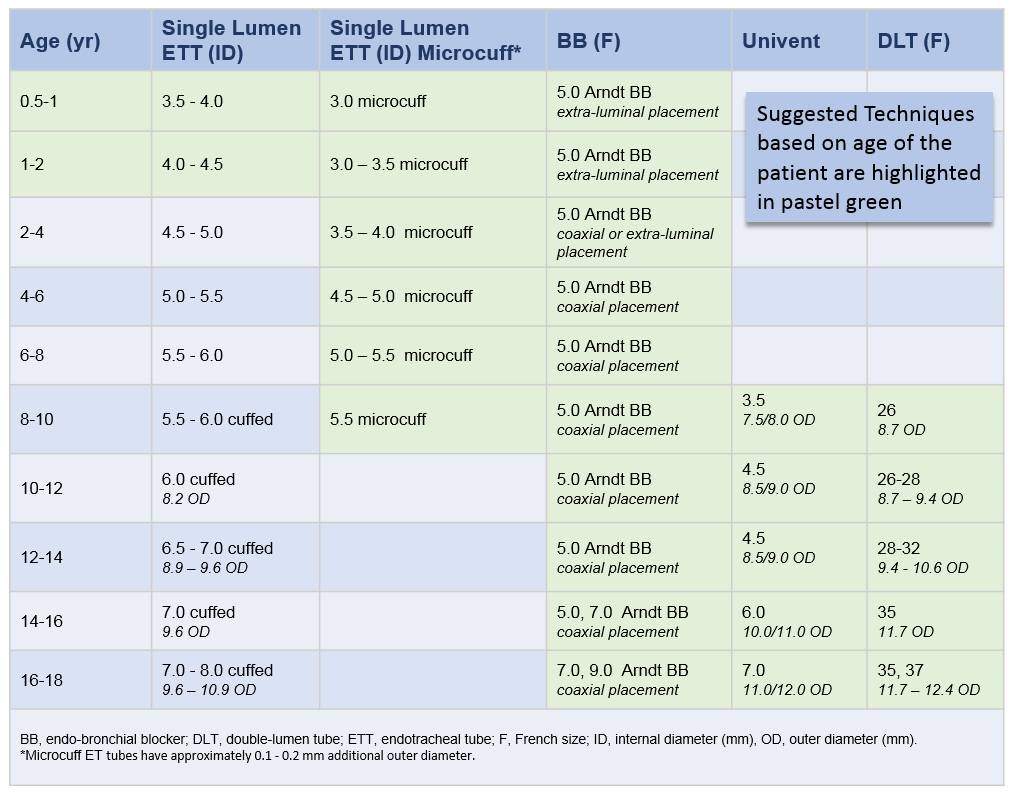
Techniques for Single-Lung Ventilation in Infants and Children
Lung isolation in infants and children can be achieved using a variety of techniques. The following section summarizes the methods in practice in our department
Single-Lumen Endotracheal Tube
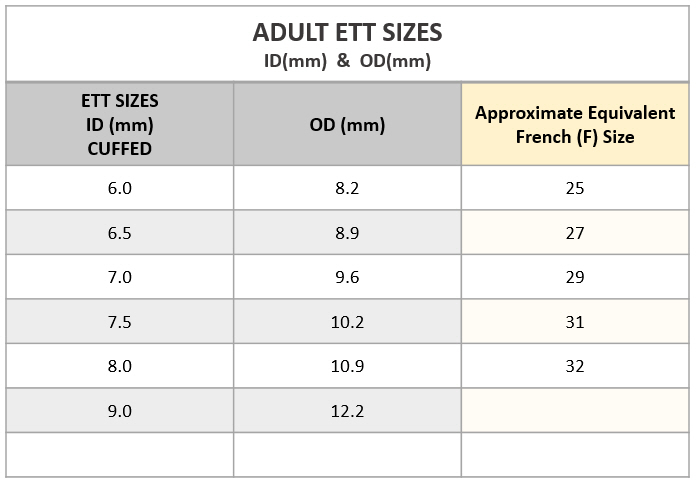
In infants and very small children (3 and under), the easiest means of providing SLV is to intentionally intubate the main stem bronchus of the non-operated lung. A pediatric bronchoscope placed through the ETT is extremely helpful in guiding and confirming accurate placement. This is particularly true when intubating the left main-stem bronchus for right sided thoracotomies. The size of the single-lumen ETT chosen should take into consideration the diameter of the main-stem bronchus and not just the trachea. An uncuffed single-lumen ETT may not provide adequate seal of the bronchus and may prevent satisfactory collapse of the operative lung . In this regard, Kimberly Clark Microcuff ETTs are a great choice. Please do note that the outer diameter (OD) of microcuff ET tubes is 0.1 - 0.2 mm larger than comparable regular uncuffed single lumen ETTs.
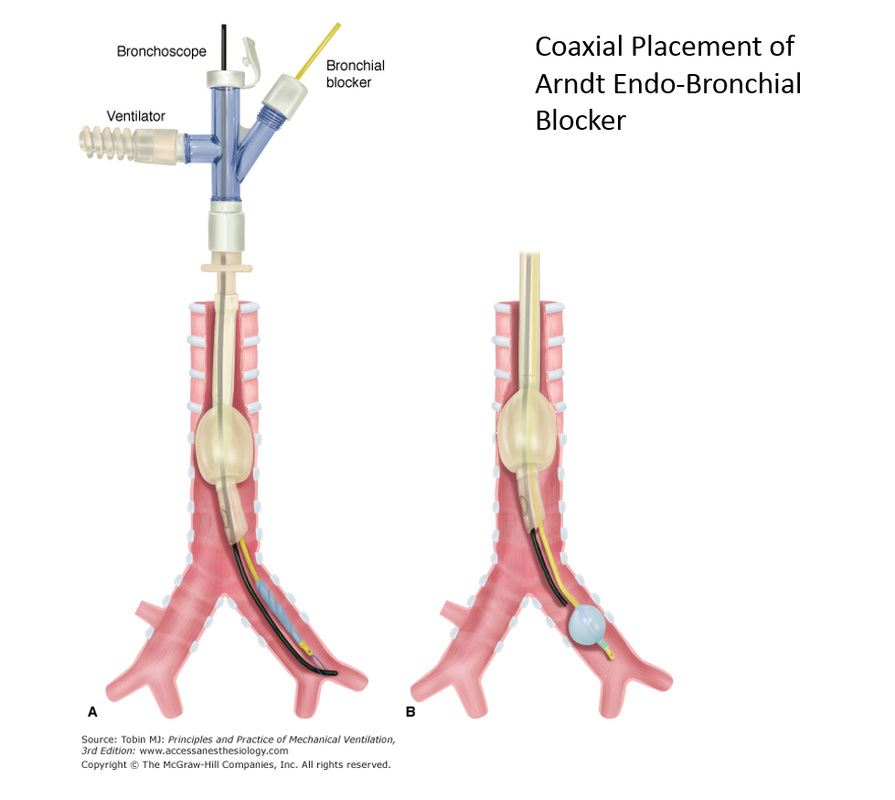
Arndt Endobrochial Blocker
The Arndt Endobronchial blocker is intended to deferentially intubate a patient's bronchus in order to isolate the left or right lung for procedures that require one-lung ventilation.
The Pediatric Arndt Endobronchial Blocker is available only in 5F size. ET tubes 4.5 ID and over can easily accommodate a 5F blocker alongside a small diameter flexible fiberoptic bronchoscope. Specialty multiport adapters are included with these kits to facilitate ventilation during placement of the blocker.
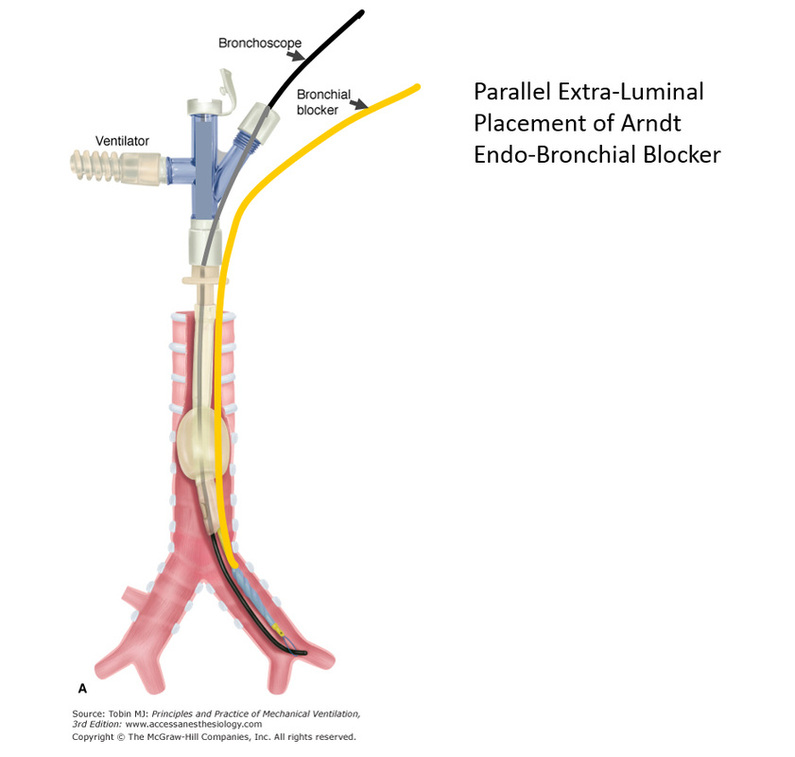
The Arndt Endobronchial blocker can be used in TWO CONFIGURATIONS depending on the age of the patient and the size of the ET tube:
1. The classical coaxial placement through the lumen of the ETT is recommended when using cuffed endotracheal tubes sizes 4.5 ID and over.
2. Parallel extra-luminal placement is recommended when using the arndt endo-bronchial blocker in infants and small children (under 24 months).
Potential Problems with Endobronchial Blockers: One potential problem with this technique is the possibility of dislodgement of the blocker balloon back into the trachea, blocking ventilation to both lungs.
The Pediatric Arndt Endobronchial Blocker is available only in 5F size. ET tubes 4.5 ID and over can easily accommodate a 5F blocker alongside a small diameter flexible fiberoptic bronchoscope. Specialty multiport adapters are included with these kits to facilitate ventilation during placement of the blocker.
The Arndt Endobronchial blocker can be used in TWO CONFIGURATIONS depending on the age of the patient and the size of the ET tube:
1. The classical coaxial placement through the lumen of the ETT is recommended when using cuffed endotracheal tubes sizes 4.5 ID and over.
2. Parallel extra-luminal placement is recommended when using the arndt endo-bronchial blocker in infants and small children (under 24 months).
Potential Problems with Endobronchial Blockers: One potential problem with this technique is the possibility of dislodgement of the blocker balloon back into the trachea, blocking ventilation to both lungs.
Univent Tube (Fuji Systems Corp)
Double Lumen Tubes
Tube Selection for Single Lung Ventilation (SLV) in Infants and Children
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023