|
|
- HOME
-
General
- About
- Pediatric Anesthesia Fellowship Program
- Pediatric Anesthesia Resident Rotation - Goals and Objectives
- Fellowship Orientation (password required)
- Fellowship Goals and Objectives
- GME Policies (password required)
- Milestones
- Revised Case Logs
- Case Minimums
- Fellow Index Cases
- Pediatric Anesthesia Certification Examination
-
Clinical Information
- What makes Pediatric Anesthesia Different?
-
Pediatric OR Setup HOME
>
- STEP-2 PEDI OR SETUP - BREATHING CIRCUIT
- STEP-3 PEDI OR SETUP - SUCTION
- STEP-4- PEDI OR SETUP - OR TABLE AND PROPS
- STEP-5- PEDI OR SETUP - MONITORS
- STEP-6 PEDI OR SETUP - AIRWAY SETUP
- STEP-7 PEDI OR SETUP - MEDICATION DESKTOP
- STEP-8 PEDI OR SETUP - IV TRAY AND LINE
- STEP-9 PEDI OR SETUP - ACCESSORIES
- STEP-10 PEDI OR SETUP - SUMMARY
- The Pediatric Anesthesia Cart
- Pediatric Normal Parameters and Equipment
- Premedication
- Drug Library
- Standard Drug Dilutions in the Pediatric OR
- Pediatric Airway Management >
- Pediatric IV Insertion Technique
- Perioperative Fluid Therapy >
- Blood Transfusion Therapy >
- Clinical Practice Guidelines
- Single Lung Ventilation (SLV) Techniques
- Regional Anesthesia >
-
PEDI STAT
- PALS ALGORITHMS
- Newborn Resuscitation Algorithm
- PALS Cardiac Arrest
- PALS Tachycardia with a pulse and poor perfusion
- PALS Bradycardia with a pulse and poor perfusion
- Cardioversion / Defibrillation
- Laryngospasm
- EZ-IO Intraosseous Infusion System
- Hyperkalemia
- Anaphylaxis
- Malignant Hyperthermia
- Society for Pediatric Anesthesia - Pedi Crisis® Critical Events Checklist
- Case Primers
- Multimedia Library
- Pediatric Anesthesia Handicraft
- Robert N Reynolds, MD Award
- Disclosure Notice
- COVID-19 RESOURCES
Glucose Requirements for Neonates and Infants
Glucose is the predominant fuel for the newborn brain and it depends on it exclusively. Hypoglycemia
(especially in the early neonatal period) predisposes to long-term
neurological damage. Normal adaptive mechanisms like
gluconeogenesis and glycogenolysis are immature in neonates and infants. Hypoglycemia is particularly of concern in the premature and sick infant. Therefore, it is important to consider intraop glucose administration in these infants. A minimum Glucose Infusion Rate (GIR) of 4-8 mg/kg/min is recommended.
Check out this GIR Calculator
Check out this GIR Calculator
Which Infants are at High Risk for Hypoglycemia
- The Preterm / Premature Infant
- IUGR, SGA, LGA infants
- Infant of a Diabetic Mother
- Sick neonates and infants (Fever, Sepsis, Respiratory Distress Syndrome (RDS), Necrotizing Enterocolitis (NEC))
- Infants on Total Parenteral Nutrition
How to Provide Basal Glucose Requirements in Neonates and Infants?
D10W and D10 1/4NS are the primary IV solutions used in neonates and young infants at risk for hypoglycemia.
These two IV solutions are also the primary IV solutions of choice to provide for hourly maintenance fluid requirements in neonates and very young infants (< 4-6 months).
Hourly Fluid Requirements calculated based on the "4-2-1 Rule" provide the minimum 5mg/kg/min of glucose needed by the infant brain.
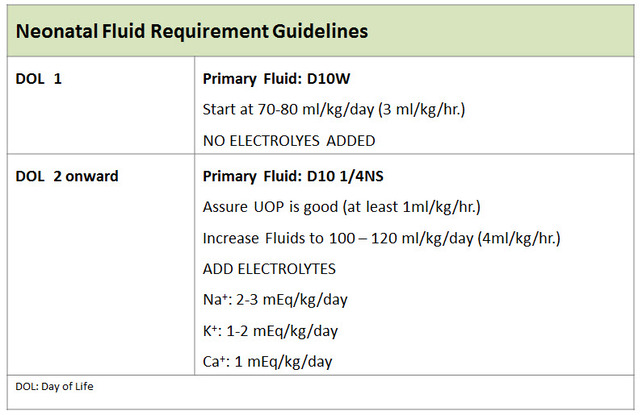
Neonates have excess total body water (TBW) at birth, which must be redistributed and excreted. Physiologic diuresis is observed during the first few days of life which results in 5-15% reduction in body weight by the end of the first week. Therefore, no electrolytes are added to hourly maintenance fluids on DOL-1 and sometimes up to DOL-2. D10W remains the primary hourly maintenance fluid on DOL-1. Thereafter as urine output (UOP) increases, maintenance rates are increased and electrolytes (Na, K, Ca) added to the maintenance fluid mix. D10 1/4NS remains the standard maintenance fluid beyond DOL-2.
Neonates and Infants who come to the OR on dextrose containing maintenance fluids should have their dextrose containing maintenance fluids continue during the case (except for brief interruptions). This will prevent intraop hypoglycemia in these patients.
These two IV solutions are also the primary IV solutions of choice to provide for hourly maintenance fluid requirements in neonates and very young infants (< 4-6 months).
Hourly Fluid Requirements calculated based on the "4-2-1 Rule" provide the minimum 5mg/kg/min of glucose needed by the infant brain.
Neonates have excess total body water (TBW) at birth, which must be redistributed and excreted. Physiologic diuresis is observed during the first few days of life which results in 5-15% reduction in body weight by the end of the first week. Therefore, no electrolytes are added to hourly maintenance fluids on DOL-1 and sometimes up to DOL-2. D10W remains the primary hourly maintenance fluid on DOL-1. Thereafter as urine output (UOP) increases, maintenance rates are increased and electrolytes (Na, K, Ca) added to the maintenance fluid mix. D10 1/4NS remains the standard maintenance fluid beyond DOL-2.
Neonates and Infants who come to the OR on dextrose containing maintenance fluids should have their dextrose containing maintenance fluids continue during the case (except for brief interruptions). This will prevent intraop hypoglycemia in these patients.
Copyright © 2014. Aman Kalra, MD Clinical Professor of Anesthesiology, Department of Anesthesiology and Perioperative Medicine (Author, Illustrator and Web Designer)
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
800 Washington Street, Box 298, Tufts Medical Center, Boston, MA 02111. USA
LAST UPDATED November 26th, 2023